Retirement Communities vs Aging in Place
Outline and How to Use This Guide
You have options, and you deserve a clear roadmap. Before we compare living models and drill down into location or lifestyle, this section sets the stage: what’s in play, what to watch for, and how to use the rest of the guide. The aim is simple—turn a complex, emotional choice into a structured process you can revisit with family, advisors, or trusted friends. Think of this as a compass: it will not choose the destination for you, but it will help you steer confidently.
First, a quick outline of what follows so you know where to find what you need:
– Section 2: A plain-English comparison of retirement communities and aging in place, including care levels, services, and typical costs.
– Section 3: Location and proximity to family and friends, with practical methods for measuring distance, travel effort, and emergency support.
– Section 4: Lifestyle preferences, from daily rhythms and hobbies to amenities, culture, and climate.
– Section 5: Costs, safety, and a decision checklist that culminates in a practical conclusion tailored to real-world choices.
How to get value from this guide:
– Skim first, decide what matters most, then return to the sections that align with your priorities.
– Print or share the checklists and questions; use them during community tours or home assessments.
– Treat money, health, and social fit as a three-legged stool; if one leg is wobbly, the whole setup can feel unstable.
Context you can use today:
– Surveys consistently show that a large majority—often around eight in ten—express a desire to remain at home. At the same time, many later report appreciating the predictability and social ease of community living once they move.
– Costs vary widely by region and by the intensity of services. Expect monthly community fees to span from modest dues for independent living to significantly higher charges when personal care or memory care is involved. Aging in place can be cost-efficient early on, but expenses may rise with home modifications and in‑home support.
– Social connection matters. Research in public health and gerontology has linked persistent isolation with higher risks for declining health; the right setting can help fortify friendships and routine contact.
Use this outline to decide what you need to read now and what can wait. The rest of the article translates trade‑offs into practical steps, so you can compare options side by side and match them to your values.
Retirement Communities vs Aging in Place: What Changes Day to Day
Retirement communities and aging in place solve the same problem—supporting a satisfying, safe later life—but they do it differently. Communities bundle housing with services and social opportunities under one roof (or campus). Aging in place keeps the household you know, while layering in modifications, neighborhood resources, and, if needed, home‑based care. The “right” answer depends less on age and more on health trajectories, budget flexibility, and appetite for maintenance or change.
What retirement communities typically offer:
– Housing designed for accessibility: single‑level layouts, elevators, and step‑free entries.
– On‑site or coordinated services: dining, transportation, housekeeping, fitness, classes, and varying levels of personal care.
– Built‑in social life: clubs, lectures, hobby rooms, gardens, and common events that make it easy to meet neighbors.
– Predictable costs: monthly fees that cover many living expenses, though care add‑ons can increase the bill.
What aging in place emphasizes:
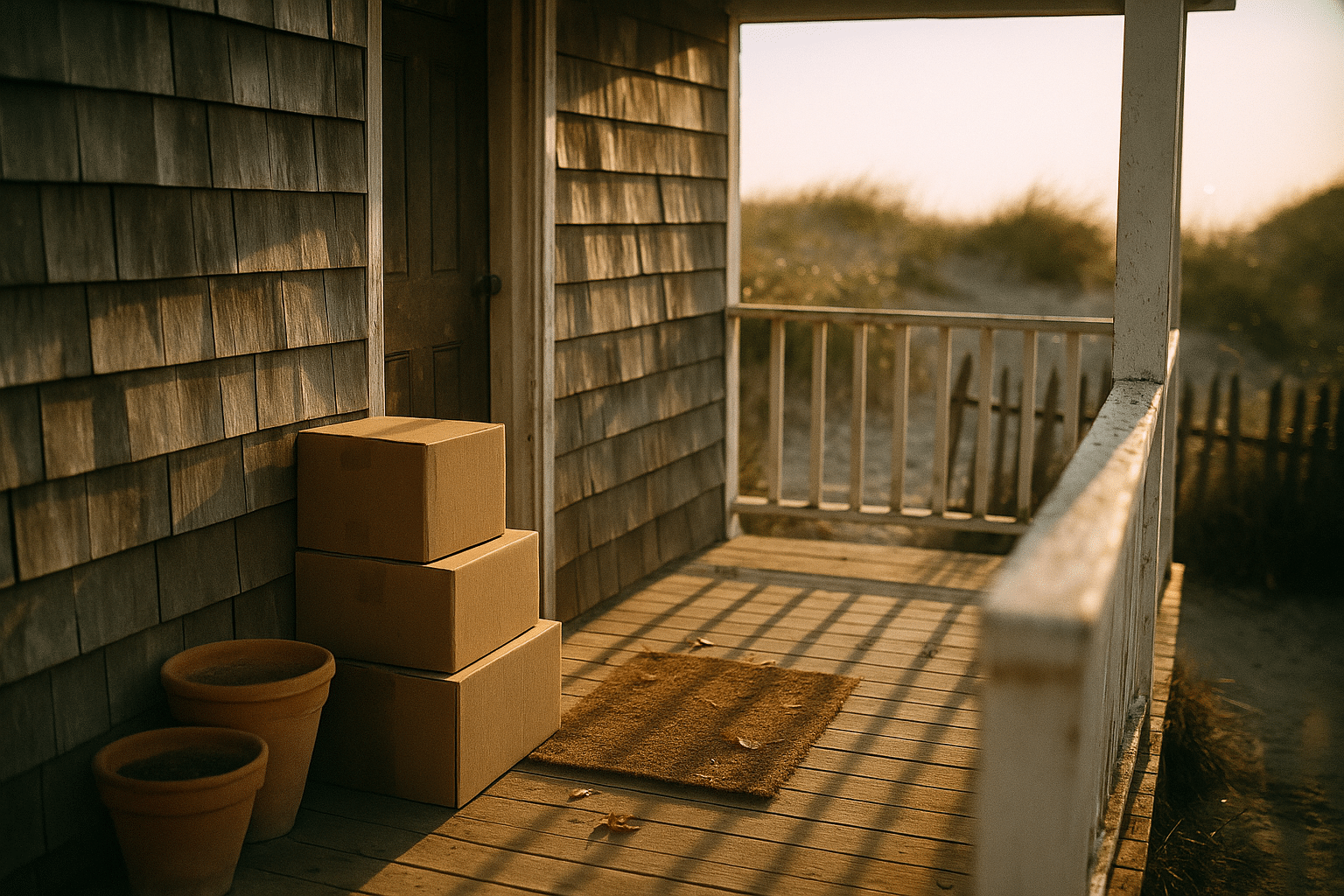
– Familiarity and control: your routines, your furniture, your kitchen, your porch.
– Custom upgrades: grab bars, zero‑threshold showers, improved lighting, wider doorways, and smart sensors for safety.
– Community assets: nearby parks, libraries, faith centers, senior centers, and volunteer networks.
– Pay‑as‑needed support: part‑time help for errands or personal care, which can scale up as needs change.
Cost dynamics in broad strokes:
– Community living often consolidates expenses (utilities, amenities, some meals) into one fee. Entry deposits may apply in some models; monthly charges rise with higher care levels.
– Staying home can be budget‑friendly if the house is paid off and care needs are light. However, ongoing maintenance, property taxes, transportation, and in‑home care hours add up, especially if round‑the‑clock support becomes necessary.
Quality‑of‑life and risk trade‑offs:
– Social vitality: communities lower barriers to connection; aging in place relies on your initiative and local network.
– Safety: communities standardize safety features; homes may need upgrades and monitoring plans.
– Flexibility: aging in place offers maximal control; communities offer convenience and a smoother path to higher care when needed.
Two quick scenarios to visualize the difference:
– Active retiree with mild arthritis: a community’s walkable campus and fitness program may reduce joint strain while keeping social life lively; aging in place works too if the home is step‑free and friends live nearby.
– Couple with one partner developing memory issues: a community with a continuum of care can simplify logistics; at home, consistent routines can be comforting but may require more caregiver coordination and respite planning.
In short, communities trade some autonomy for convenience and social ease; aging in place trades convenience for control and familiarity. Both can work beautifully when matched to the right needs and supports.
Location and Proximity to Family and Friends
Where you live shapes how often you see people, how quickly help arrives, and how easily you stay involved in daily life. Distance on a map is only part of the equation; time and effort matter more. A ten‑mile drive across town during rush hour can be harder than a forty‑minute off‑peak trip from a nearby suburb. Flight schedules, winter weather, and the availability of public transit or ride services all influence whether visits feel casual or complicated.
How to measure proximity realistically:
– Convert miles into minutes across different times of day; test the route you and your visitors will take.
– Map “care radius” resources: hospitals, urgent care, pharmacies, and groceries, noting typical wait times and peak hours.
– Consider caregiver convenience: can adult children or close friends fit visits into their routines without rearranging everything?
– Factor in travel resilience: if stairs or long walks are tiring, even a short distance can become a barrier without good access.
Social connection is more than company; it’s a buffer against isolation. Large studies have linked chronic loneliness to elevated risks for declining health and delayed recovery. The remedy isn’t simply “moving closer”; it’s ensuring regular, low‑friction contact. A small apartment five minutes from a grandchild’s school might lead to more drop‑ins than a larger home thirty miles away. Similarly, a community that places you near peers who share your interests can transform occasional chats into genuine friendships.
Regional realities matter:
– Climate: snow and ice complicate winter driving and walking; extreme heat can limit outdoor time and strain energy.
– Terrain and walkability: sidewalks, crosswalk timing, benches, and lighting influence how often you step outside.
– Culture: some towns are organized around neighborhood clubs and volunteerism; others lean on family networks or faith communities.
– Cost of living: being near family in a high‑cost city may strain a budget; a nearby but more affordable town might strike a better balance.
Practical tests before you decide:
– Spend a week in the area, mimic your routine, and note how easy it is to meet a friend for coffee, attend a class, or see a doctor.
– Time an urgent‑care run during a typical busy hour; a fifteen‑minute goal from door to door is a useful benchmark for peace of mind.
– Ask loved ones to commit to specific visit patterns (“Sundays for dinner,” “Wednesdays for errands”). Predictable schedules reduce emotional guesswork.
The right location shrinks the distance between intention and action. When visits are easy and services are close, connection becomes habit rather than a special occasion—and that can make all the difference.
Lifestyle Preferences: Routines, Activities, and Personal Fit
Homes and communities are more than addresses; they’re stage sets for daily life. Start with the rhythms that make you feel like yourself—morning coffee at a sunny window, a weekly choir rehearsal, a brisk walk before dinner, or quiet afternoons with a novel and a cat on your lap. The ideal setting reinforces those habits rather than fighting them. When the environment fits your routine, motivation comes more easily and well‑being follows.
Questions to calibrate your lifestyle:
– How much structured activity feels energizing versus overwhelming?
– Do you prefer spontaneous gatherings or planned events?
– What hobbies require space or equipment (gardening beds, workshop benches, an art studio)?
– Are pets central to your day, and what policies or yard space will they need?
– How sensitive are you to noise, hallway traffic, or late‑night lights?
In retirement communities, amenities reduce friction:
– Fitness centers, pools, and walking loops minimize travel to exercise.
– Classes, clubs, and lectures put social opportunities on the calendar without coordination.
– Dining options simplify nutrition and cleanup, which can be especially helpful during low‑energy days.
– Transportation services turn errands into brief outings rather than logistical puzzles.
At home, lifestyle is tailored by you:
– You can design spaces around your hobbies: raised garden beds, a converted workshop corner, or a quiet reading nook with adjustable lighting.
– You choose the soundtrack: birds in the yard, jazz in the kitchen, or nighttime silence.
– Local resources fill gaps: library programs, senior centers, park walking groups, and nearby volunteer opportunities.
Consider climate and seasons. If winter cabin fever sets in, a community with indoor amenities can keep you active; alternatively, a home near a walkable town center might supply year‑round stimulation. Light and greenery matter, too; sunlight in the breakfast room or a tree‑lined path outside the front door can have outsized effects on mood and consistency.
Finally, think about identity and belonging. Do you want a diverse environment with many viewpoints or a familiar culture that mirrors your own traditions? Are intergenerational interactions important, or do you prefer a quieter, age‑restricted setting? Trial experiences help: take a class, join a community dinner, or shadow a typical day. The place that supports your favorite version of yourself is likely the one you’ll stick with—and enjoy.
Costs, Safety, and a Practical Decision Checklist (Conclusion)
Money, safety, and planning tie everything together. A sensible budget compares apples to apples: housing costs, utilities, meals, transportation, maintenance, insurance, taxes, and out‑of‑pocket care. In a community, many of these roll into a monthly fee, with higher charges for added personal care. At home, individual line items can start low but may spike if mobility changes or if overnight help becomes necessary. A realistic forecast models multiple scenarios rather than a single “average” year.
Cost and safety checkpoints:
– Home upgrades: factor in grab bars, step‑free entries, bathroom renovations, brighter lighting, and smoke/CO detectors with alerts.
– Transportation: plan for the day you drive less; price ride services, shuttles, or delivery memberships.
– Care hours: compare rates for part‑time help versus full‑time or live‑in support; the difference is substantial.
– Emergency access: time the route to urgent care and note after‑hours options.
– Insurance and contingencies: understand coverage for rehabilitation, home care, or residential services, and set aside an emergency fund.
Decision checklist to finalize your path:
– List your top five priorities (for example: social life, walkability, budget ceiling, nearby family, pet space) and rank them.
– Score each option from 1–5 against those priorities; a simple grid reveals strengths and trade‑offs.
– Stress‑test the future: picture a fall, a medical flare, or a partner needing more help—does your plan bend without breaking?
– Pilot the choice: try short‑term stays, extended visits, or seasonal rentals before committing.
– Involve your circle: invite two trusted people to challenge assumptions and spot blind spots.
Summary for readers weighing this decision now: retirement communities streamline daily living and activate social life, trading some control for convenience and a smoother path to higher care. Aging in place preserves autonomy and the comfort of home, but demands more coordination and may become costlier as needs intensify. The right answer aligns budget, safety, and identity. Start with priorities, verify them with a small pilot, and choose the setting that makes the good days easy and the tough days manageable. That is a grounded, sustainable plan you can feel confident about.